Symptoms
Spider veins
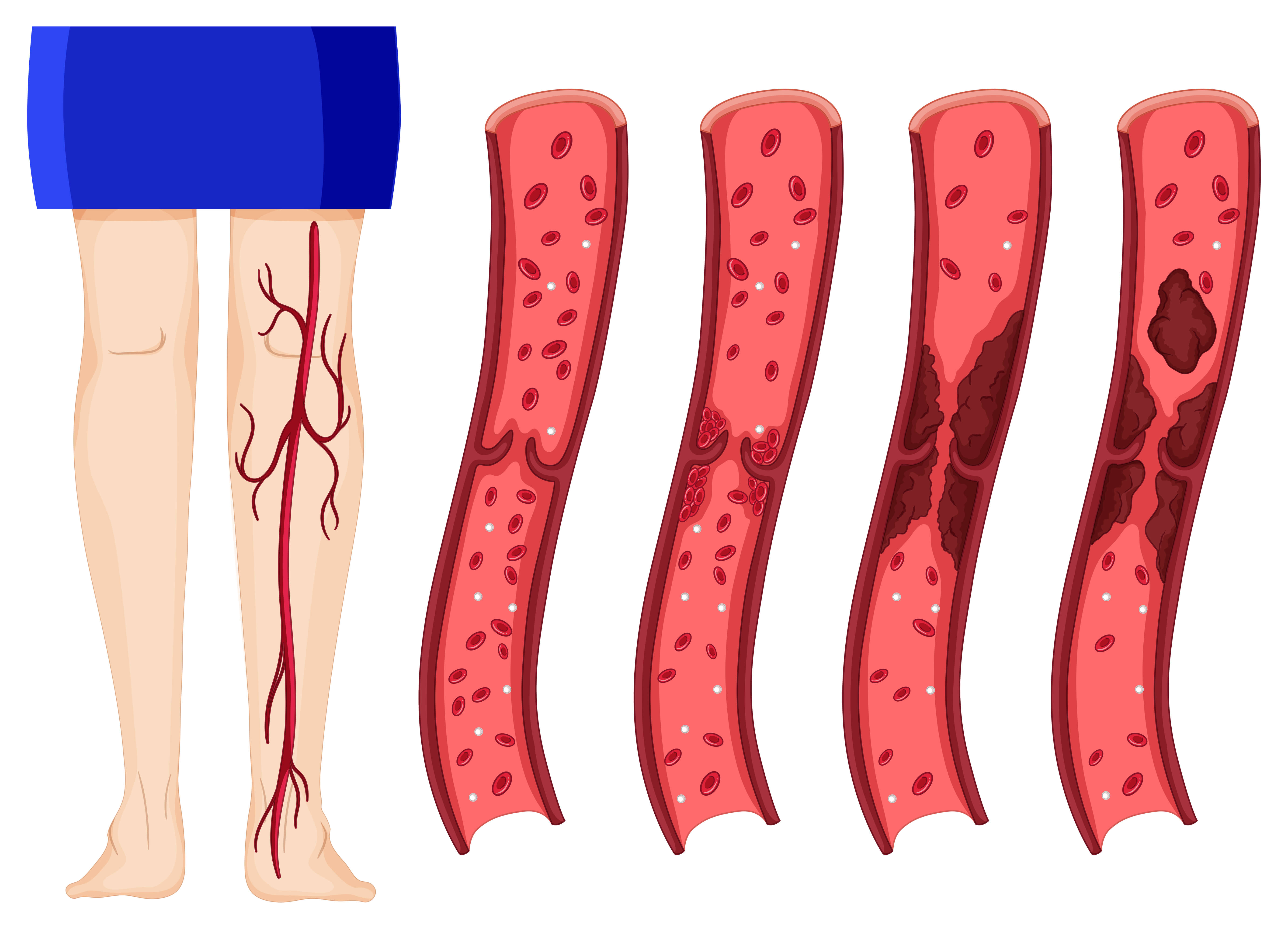
Varicose veins might not cause pain. Signs of varicose veins include:
Veins that are dark purple or blue
Veins that appear twisted and bulging, often appearing like cords on the legs
When painful signs and symptoms of varicose veins occur, they might include:
An achy or heavy feeling in the legs
Burning, throbbing, muscle cramping and swelling in the lower legs
Worsened pain after sitting or standing for a long time
Itching around one or more of the veins
Changes in skin color around a varicose vein
Spider veins are similar to varicose veins, but they're smaller. Spider veins are found closer to the skin's surface and are often red or blue.
Spider veins occur on the legs but can also be found on the face. They vary in size and often look like a spider's web.
When to see a doctor
If you're concerned about how your veins look and feel and self-care measures haven't helped, see your health care provider.
Diagnosis
Your health care provider will do a physical exam, including looking at your legs while you're standing to check for swelling. Your provider might also ask you to describe pain and aching in your legs.
Tests
To diagnose varicose veins, a health care provider might recommend a test called a venous Doppler ultrasound of the leg. A Doppler ultrasound is a noninvasive test that uses sound waves to look at blood flow through the valves in the veins. A leg ultrasound can help detect a blood clot.
In this test, a health care provider moves a small hand-held device (transducer), which is about the size of a bar of soap, against the skin over the body area being examined. The transducer transmits images of the veins in the legs to a monitor, which displays the results.
Treatment
Treatment for varicose veins may include self-care measures, compression stockings, and surgeries or procedures. Procedures to treat varicose veins are often done as an outpatient procedure, which means you usually go home on the same day.
Self-care
Self-care — such as exercise, raising the legs when sitting or lying down, or wearing compression stockings — can help ease the pain of varicose veins and might prevent them from getting worse.
Compression stockings
Wearing compression stockings all day is often the first approach to try. The stockings squeeze the legs, helping veins and leg muscles move blood more efficiently. The amount of compression varies by type and brand.
Compression stockings are available at most pharmacies and medical supply stores. Prescription-strength stockings also are available and may be covered by insurance if varicose veins are causing symptoms.
Surgeries or other procedures
If self-care steps and compression stockings don't work, or varicose veins are more severe, a health care provider might recommend surgery or other procedures:
Sclerotherapy : A health care provider injects the varicose veins with a solution or foam that scars and closes those veins. In a few weeks, treated varicose veins should fade.
The same vein might need to be injected more than once. Sclerotherapy doesn't require anesthesia and can be done in a health care provider's office.
Laser treatment : Laser treatment sends strong bursts of light onto the vein, which makes the vein slowly fade and disappear. No cuts or needles are used.
Catheter-based procedures using radiofrequency or laser energy : This procedure is the preferred treatment for larger varicose veins. A health care provider inserts a thin tube (catheter) into an enlarged vein and heats the tip of the catheter using either radiofrequency or laser energy. As the catheter is removed, the heat destroys the vein by causing it to collapse and seal shut.
High ligation and vein stripping : This procedure involves tying off a vein before it joins a deep vein and removing the vein through small cuts. This is an outpatient procedure for most people. Removing the vein won't keep blood from flowing in the leg because veins deeper in the leg take care of the larger volumes of blood.
Ambulatory phlebectomy (fluh-BEK-tuh-me) : A health care provider removes smaller varicose veins through a series of tiny skin punctures. Only the parts of the leg that are being pricked are numbed in this outpatient procedure. Scarring is generally minimal.